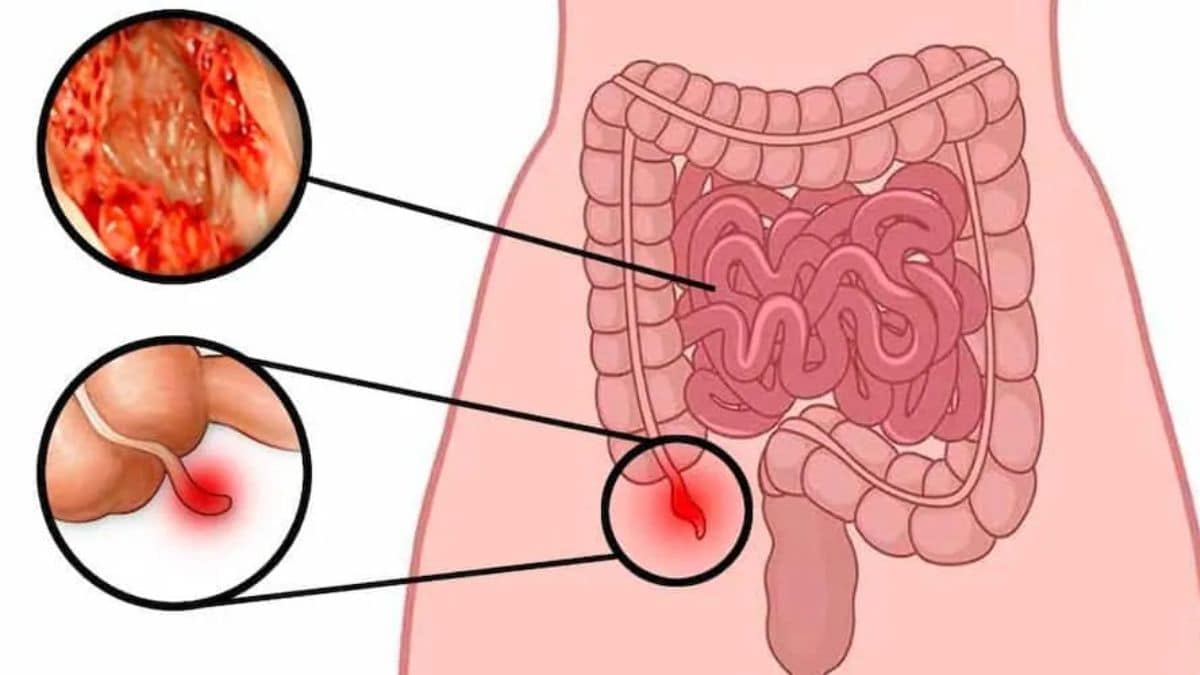
Once considered extremely rare, appendix cancer is now showing a worrying rise particularly among younger adults. New research suggests that cases have quadrupled in recent decades with many detected at advanced stages due to vague or absent symptoms. As awareness remains low and early detection difficult, understanding the signs, risk factors and treatment pathways becomes critical.
Firstpost spoke to Dr Amit Javed, Senior Director – GI & GI Oncology, Fortis Hospital (Gurugram) to understand why appendix cancer is on the rise, how it presents clinically and what can be done to improve outcomes.
Why are appendix cancer cases rising among younger adults, particularly millennials and Gen Z?
Dr Amit: While appendiceal cancer remains a relatively rare malignancy, there has been a noticeable increase in diagnoses among younger adults in recent years. This trend, similar to what has been observed in early-onset colorectal cancers, may be attributed to a combination of improved diagnostic capabilities and changing risk factors. Advanced imaging techniques, greater use of diagnostic laparoscopy, and more frequent appendectomies for non-specific abdominal pain have likely led to increased incidental detection of early-stage appendiceal tumors.
However, this alone may not fully explain the shift in age demographics. Emerging research suggests that shifts in gut microbiota, rising obesity rates, dietary patterns rich in processed foods, sedentary lifestyles, and possible environmental exposures may be influencing cancer biology in younger cohorts. More data is needed to conclusively identify causative links, but the trend is certainly being observed across high-resource healthcare settings.
Is there a known link between appendix cancer and lifestyle, genetics or environmental exposures in younger populations?
Dr Amit: Currently, there is no single established cause of appendix cancer. However, certain associations are being actively studied:
•Lifestyle Factors: Diets high in red or processed meats, low fibre intake, and obesity known contributors to colorectal cancer may also play a role in appendix malignancies, though data is limited.
•Environmental Exposures: Exposure to microplastics, industrial chemicals, and endocrine-disrupting substances may influence carcinogenesis in the gastrointestinal tract, including the appendix. However, this is still an area of ongoing investigation.
•Genetic Predisposition: Some appendiceal tumours may be associated with Lynch syndrome or familial cancer syndromes, though far less commonly than colorectal cancer. Molecular profiling is now recommended in many cases to evaluate for potential hereditary links.
In most young patients, appendix cancer appears sporadic, but the rising numbers point toward the need for deeper evaluation of modern environmental and epigenetic influences.
Given that appendix cancer is often detected late due to vague symptoms, what early signs should individuals especially young adults watch out for?
Dr Amit: Appendix cancer often presents with non-specific symptoms, making early detection challenging. In younger adults, the following signs should prompt medical evaluation:
•Persistent or recurrent right lower abdominal pain, especially if similar to appendicitis but not resolving
•Unexplained abdominal bloating or distension
•Altered bowel habits without an identifiable cause
•Unintended weight loss, fatigue, or anemia
•A palpable mass or fullness in the lower abdomen
In many cases, appendiceal tumours are incidentally discovered during appendectomy for presumed acute appendicitis. This underlines the importance of histopathological analysis of every appendectomy specimen, even in young patients.
How is appendix cancer different, genetically and clinically from other gastrointestinal cancers such as colon or rectal cancer?
Dr Amit: Appendix cancer is a biologically and clinically distinct entity from colorectal malignancies. It encompasses several histologic subtypes, including:
•Neuroendocrine tumours (NETs)
•Mucinous adenocarcinomas
•Goblet cell carcinoids
•Signet ring cell carcinomas
Each of these has unique behaviour, prognosis, and treatment pathways.
Genetically, appendix tumours may harbour different molecular signatures, including variations in KRAS, GNAS, and TP53 mutations, particularly in mucinous tumours. Unlike colorectal cancers, microsatellite instability (MSI) and APC mutations are less common.
Clinically, mucinous tumours can produce large amounts of mucin, sometimes leading to pseudomyxoma peritonei (PMP) — a condition rarely seen in other GI cancers. Treatment and surveillance strategies are therefore quite different.
Can you walk us through how appendix cancer is typically diagnosed and staged? Are there improvements in imaging or biomarkers that aid in earlier detection?
Dr Amit: Diagnosis often begins incidentally during surgery for suspected appendicitis. If a tumour is suspected pre-operatively, the following steps are involved:
Imaging:
•Contrast-enhanced CT scans remain the mainstay for detecting masses, mucinous ascites, or peritoneal spread.
•MRI with diffusion-weighted imaging is increasingly used, particularly for mucinous tumours, to better characterise peritoneal involvement.
•PET-CT may be helpful in certain subtypes, especially aggressive variants or high-grade neuroendocrine tumours.
Tumour Markers:
•CEA, CA 19-9, and CA-125 may be elevated in mucinous appendiceal cancers, although they are not diagnostic and are mainly used for monitoring.
•Histopathology and Immunohistochemistry:
•Once the appendix is removed, detailed pathological examination is essential to classify the tumour type, grade, and margins.
Staging:
•Staging follows the AJCC TNM system, but peritoneal cancer index (PCI) scoring is also critical in cases involving peritoneal spread to guide surgical decision-making.
While no single biomarker currently allows for early non-invasive detection, research is ongoing into liquid biopsy and circulating tumour DNA (ctDNA) for earlier diagnosis and monitoring.
What are the current treatment options available for appendix cancer? How effective are newer approaches like HIPEC (Hyperthermic Intraperitoneal Chemotherapy)?
Dr Amit: Treatment depends heavily on the tumour histology, grade, and extent of spread:
•Localised tumours (e.g., small neuroendocrine tumours <2 cm) may be treated with appendectomy alone.
•Larger or invasive tumours typically require a right hemicolectomy to ensure adequate lymph node clearance.
•Mucinous tumours with peritoneal dissemination or PMP are managed with:
•Cytoreductive surgery (CRS) — complete surgical removal of visible tumour
•Followed by HIPEC — heated chemotherapy circulated in the abdomen to target microscopic residual disease
HIPEC has revolutionized survival outcomes in selected patients with peritoneal spread, offering long-term survival and in some cases, cure particularly when performed in high-volume centers with surgical expertise.
•Systemic chemotherapy is used selectively in high-grade tumours or inoperable cases, often with regimens similar to colorectal cancer.
Do you see a need for changes in screening guidelines or increased awareness in primary care to address this rise in younger patients?
Dr Amit: Given the rarity and variable presentation of appendix cancer, routine population-based screening is not currently recommended.
However, there is a growing need for:
•Greater awareness among primary care physicians and emergency practitioners to consider malignancy in atypical or recurrent abdominal pain, especially in younger patients
•Routine histopathological examination of all appendectomy specimens, regardless of patient age
•Genetic counselling and testing in young patients with aggressive or familial patterns of disease
•Investment in biobanking and molecular profiling to better understand early-onset GI cancers, including appendiceal tumours
As trends evolve, surveillance strategies may eventually be tailored for higher-risk populations, especially if environmental or genetic risk markers are identified in the future.